2025: All Medi-Cal Must Be In Managed Care
2025: All Medi-Cal Must Be in Managed Care
Related Articles: 2025: All Medi-Cal Must Be in Managed Care
- 2025 Chevrolet Suburban: The Epitome Of American Full-Size SUVs
- What Year Are We In? 2025: A Glimpse Into The Future
- XRP Price Forecast 2050: A Comprehensive Analysis
- U S Open Golf 2025
- The New 2024 Nissan GT-R: Unveiling The Beast
Introduction
With great pleasure, we will explore the intriguing topic related to 2025: All Medi-Cal Must Be in Managed Care. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Video about 2025: All Medi-Cal Must Be in Managed Care
2025: All Medi-Cal Must Be in Managed Care
Introduction
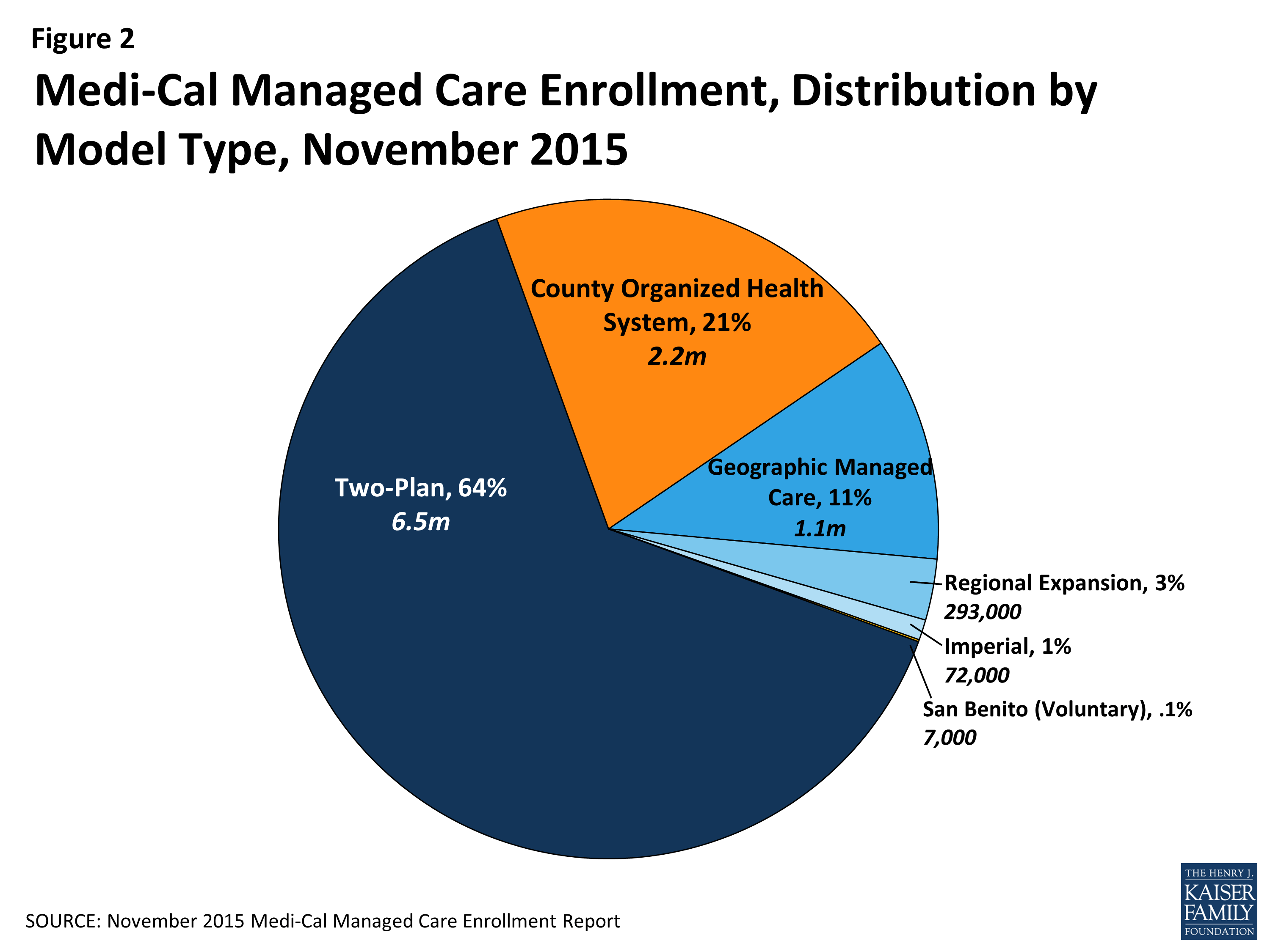
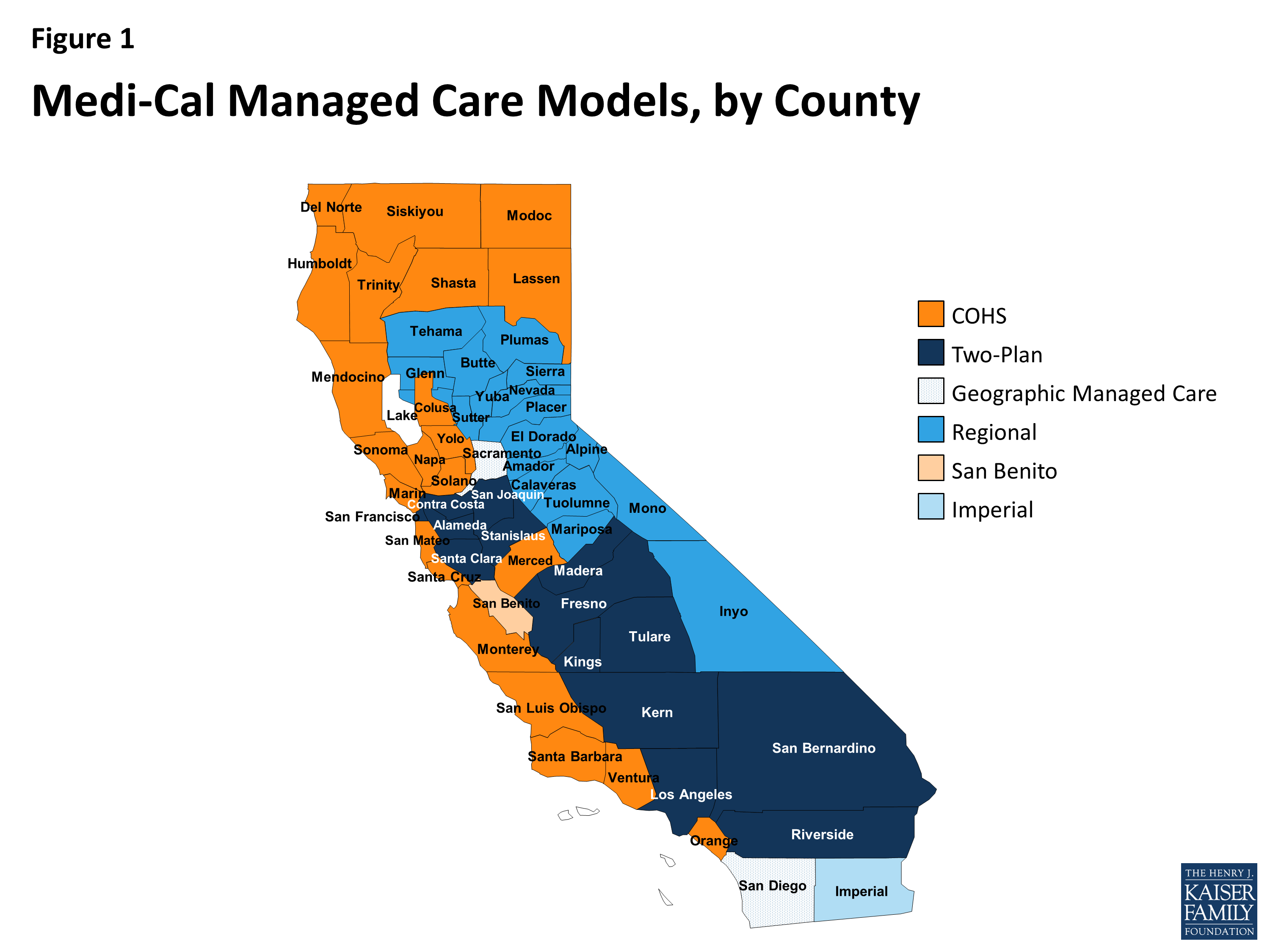
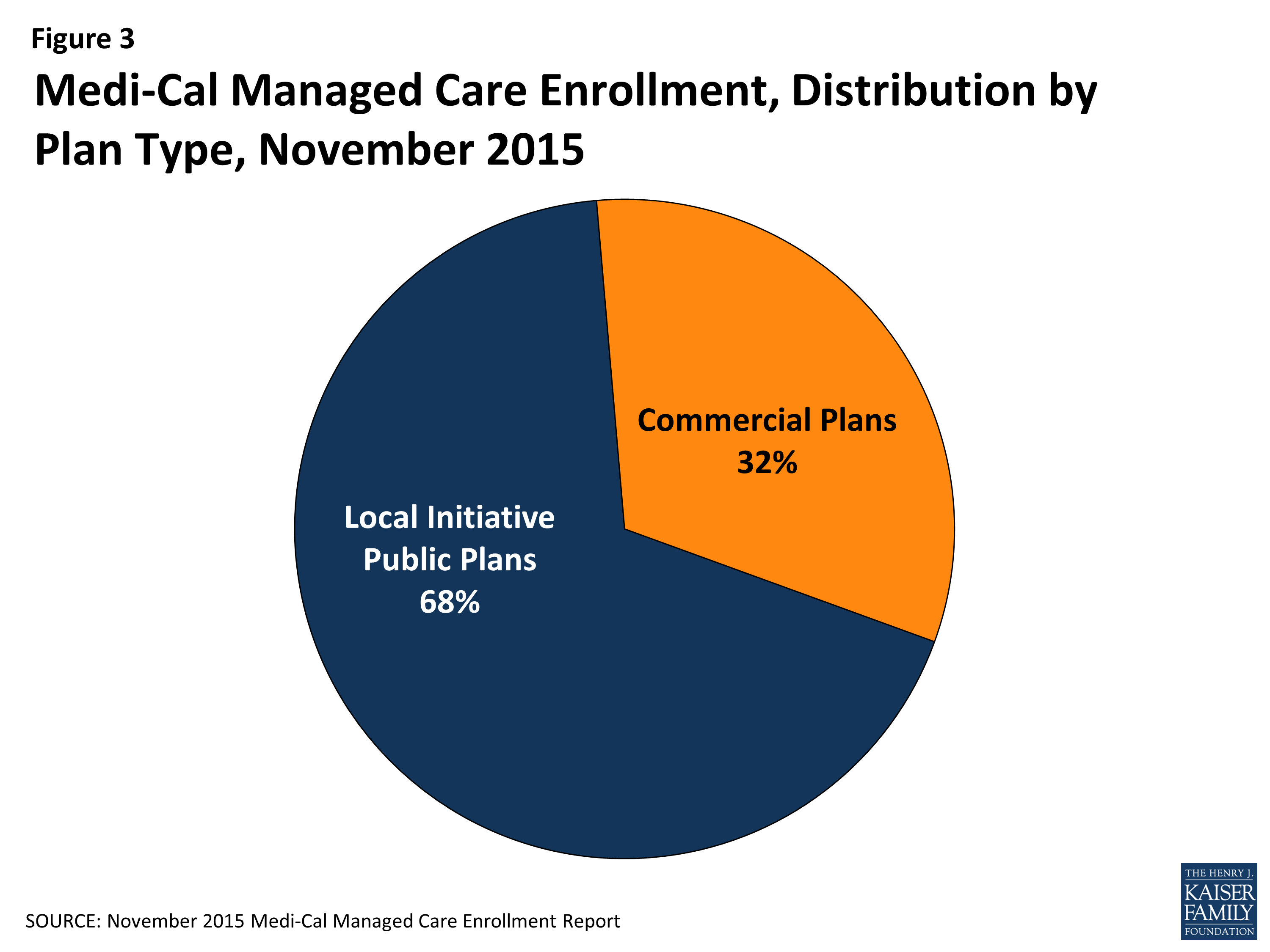
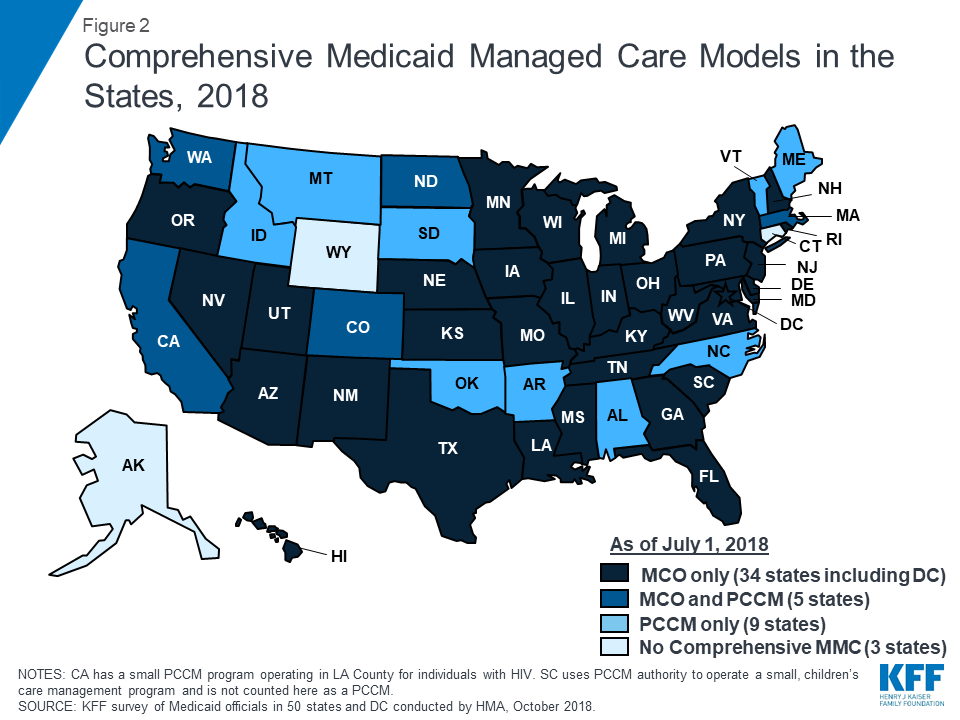
Medi-Cal, California’s Medicaid program, provides health insurance to low-income individuals and families. Currently, about 80% of Medi-Cal beneficiaries are enrolled in managed care plans, which contract with the state to provide comprehensive health care services. The remaining 20% of beneficiaries are enrolled in fee-for-service (FFS) Medi-Cal, which allows them to see any provider who accepts Medi-Cal.
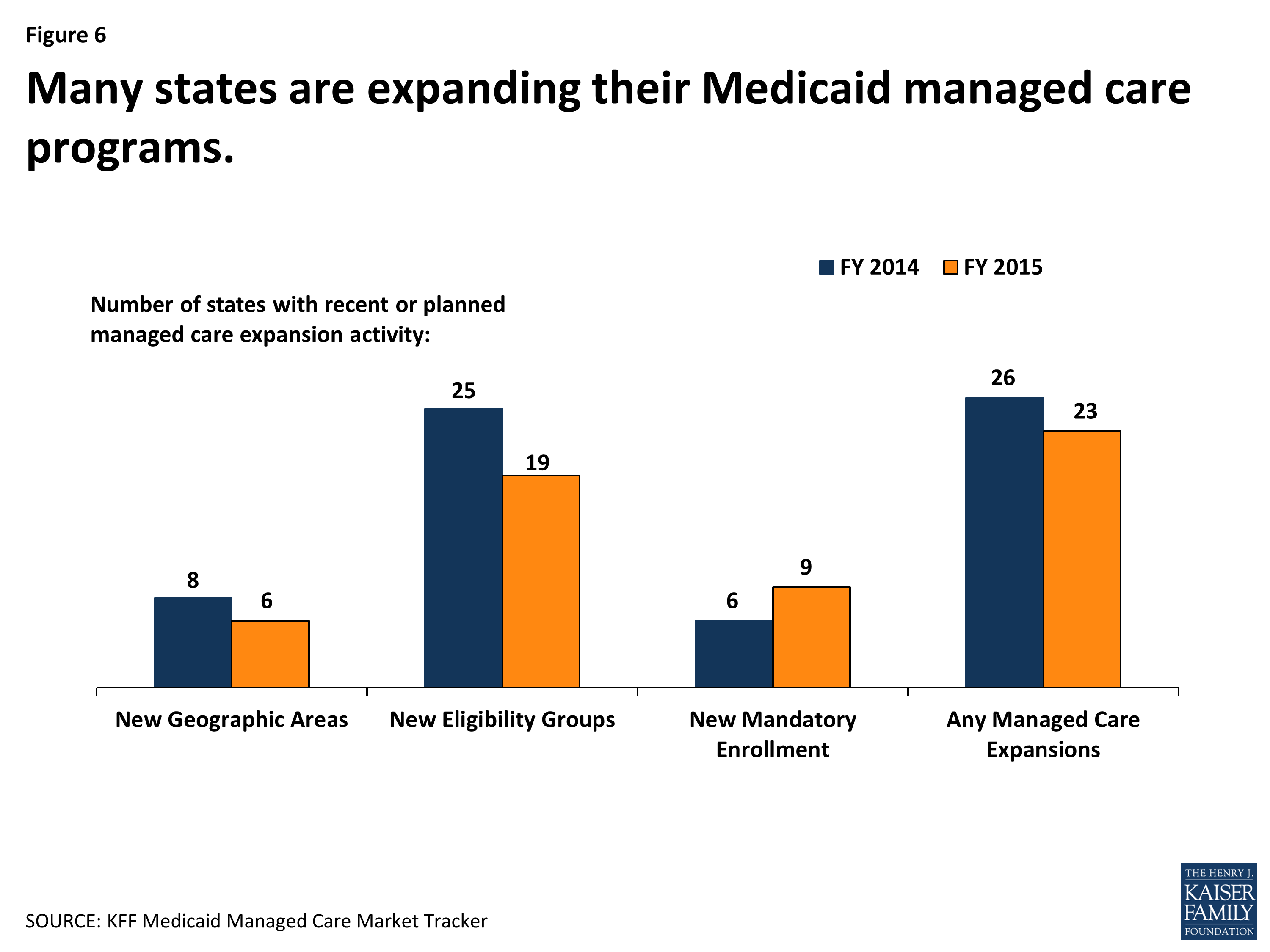
In 2021, the California Legislature passed Assembly Bill 133, which requires all Medi-Cal beneficiaries to be enrolled in managed care plans by January 1, 2025. This is a significant change to the Medi-Cal program, and it has the potential to improve the quality of care for beneficiaries while reducing costs.
Benefits of Managed Care
Managed care plans offer a number of benefits over FFS Medi-Cal, including:
- Improved coordination of care: Managed care plans have a team of care coordinators who work with beneficiaries to develop a personalized care plan. This can help to ensure that beneficiaries receive all of the services they need, and it can also help to prevent unnecessary duplication of services.
- Lower costs: Managed care plans are able to negotiate lower rates with providers, which can save the state money. In addition, managed care plans can help to reduce the number of unnecessary hospitalizations and emergency room visits, which can also save money.
- Better quality of care: Managed care plans are required to meet certain quality standards, which helps to ensure that beneficiaries receive high-quality care. In addition, managed care plans often offer a wider range of services than FFS Medi-Cal, which can make it easier for beneficiaries to get the care they need.
Challenges of Transitioning to Managed Care
While managed care offers a number of benefits, there are also some challenges associated with transitioning to a fully managed care system. These challenges include:
- Loss of choice: Beneficiaries who are currently enrolled in FFS Medi-Cal will lose the ability to see any provider who accepts Medi-Cal. Instead, they will be required to choose a managed care plan. This could be a significant inconvenience for some beneficiaries, especially those who have established relationships with their current providers.
- Access to care: Some beneficiaries may have difficulty accessing care under managed care. This could be due to a number of factors, such as the availability of providers in their area or the plan’s rules and regulations.
- Disruption of care: Transitioning to managed care can be disruptive for beneficiaries. They may have to change providers, and they may have to learn a new system of care. This can be especially challenging for beneficiaries with complex medical needs.
The Path Forward
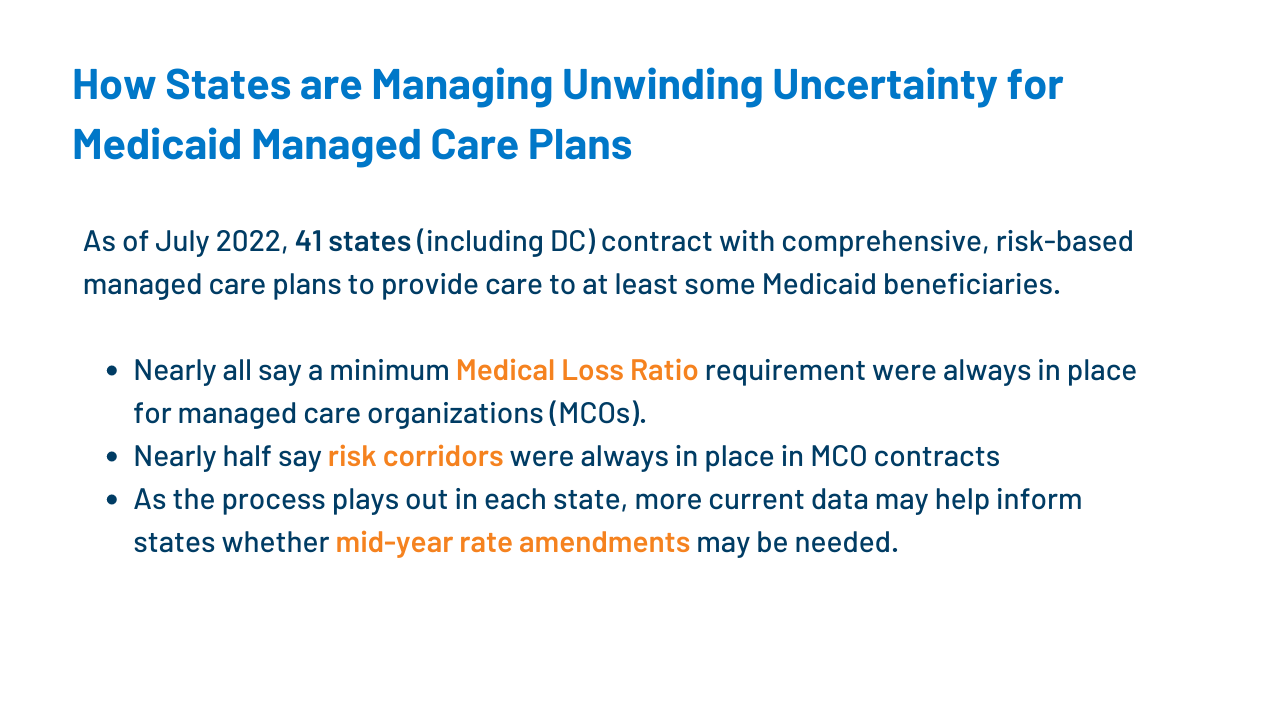
The California Department of Health Care Services (DHCS) is working to ensure a smooth transition to managed care for all Medi-Cal beneficiaries. DHCS is working with managed care plans to develop and implement new programs and services that will meet the needs of beneficiaries. DHCS is also working to educate beneficiaries about the changes to the Medi-Cal program and to help them choose a managed care plan that is right for them.
The transition to managed care is a major change to the Medi-Cal program, but it has the potential to improve the quality of care for beneficiaries while reducing costs. DHCS is committed to working with managed care plans and beneficiaries to ensure a smooth and successful transition.
Conclusion
The transition to managed care for all Medi-Cal beneficiaries is a significant change to the program, but it is one that has the potential to improve the quality of care for beneficiaries while reducing costs. DHCS is working to ensure a smooth and successful transition, and it is committed to working with managed care plans and beneficiaries to ensure that all beneficiaries have access to the care they need.


Closure
Thus, we hope this article has provided valuable insights into 2025: All Medi-Cal Must Be in Managed Care. We thank you for taking the time to read this article. See you in our next article!